About 30% of people with IBS also have lactose intolerance, which can make figuring out your gut issues feel like solving a mystery. You may notice bloating, cramps, or diarrhea after eating dairy, but is it IBS acting up or just your body rejecting lactose? The symptoms overlap, but the causes and fixes aren’t the same—and understanding the difference could change how you handle meals. Let’s analyze what sets them apart so you can find relief without guessing.
Shared Symptoms of IBS and Lactose Intolerance
Should you’ve ever felt bloated or gassy after eating, you could question whether it’s IBS or lactose intolerance—especially since both can leave you rushing to the bathroom.
The overlapping symptoms make it tricky to tell them apart. With lactose intolerance, your digestive system struggles to digest lactose, causing gas, cramps, and diarrhea within hours of eating dairy.
IBS shares these discomforts but isn’t always tied to specific foods—stress or other triggers could set it off. Both conditions mess with your gut, leaving you uneasy after meals.
Dietary changes can help, like cutting out lactose or identifying IBS triggers, but pinpointing the cause matters. Should symptoms linger, a doctor can help sort it out.
Either way, you’re not alone—millions deal with these digestive woes daily.
Distinct Symptoms That Set IBS Apart
Since bloating and bathroom trips can point to either IBS or lactose intolerance, it helps to know the telltale signs that set IBS apart.
Unlike lactose intolerance, which flares up in instances where you lack the enzyme lactase to digest dairy, IBS triggers abdominal pain linked to stress or multiple dietary triggers—not just lactose. The pain often eases after bowel movements, and you could notice mucus in your stool, which isn’t common with lactose issues.
IBS can also swing between constipation and diarrhea, while lactose intolerance usually causes diarrhea alone. Your doctor might use the Rome IV criteria to diagnose IBS, focusing on how often and intensely your belly hurts.
These distinctions clarify whether it’s IBS or just trouble digesting dairy.
Unique Symptoms of Lactose Intolerance
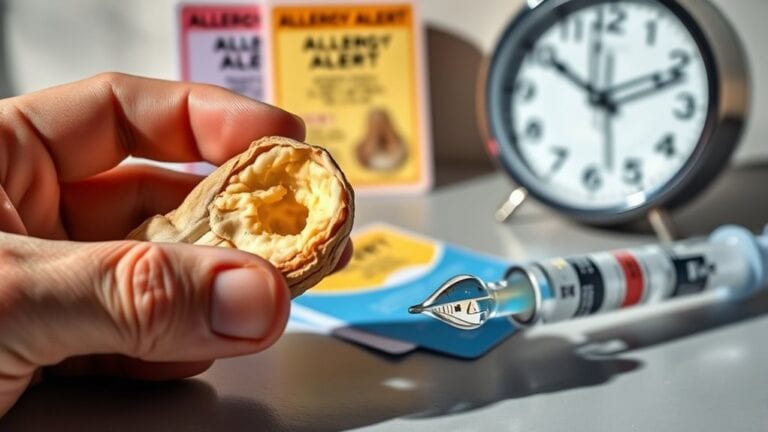
Ever contemplated why that bowl of ice cream leaves you bloated and rushing to the bathroom?
Should that be the case, you could be experiencing the unique symptoms of lactose intolerance. Unlike IBS, these issues kick in fast—usually within 30 minutes to 2 hours after eating dairy products. Undigested lactose ferments in your gut, causing gas and bloating that can feel downright miserable.
You may also deal with diarrhea, nausea, or even vomiting, all because your body struggles to digest lactose. The triggers are clear-cut: milk, cheese, or ice cream are often the culprits.
While IBS symptoms overlap, lactose intolerance is directly tied to dairy. Should cutting back on these foods ease your discomfort, you’ve likely pinpointed the problem.
Causes and Risk Factors for IBS
You may ponder what causes IBS, and while experts aren’t entirely sure, they’ve found that miscommunication between your gut and brain can play a big role.
Certain foods, stress, or even past infections could trigger or worsen your symptoms, making your digestive system extra sensitive.
Changes in your gut bacteria could also contribute, leaving you feeling out of balance.
Gut-Brain Communication Issues
Should your gut feel like it’s sending mixed signals, you’re not imagining it—miscommunication between your brain and digestive system is a big reason behind irritable bowel syndrome (IBS). As gut-brain communication gets disrupted, your intestines might overreact or underreact, leading to pain, bloating, or altered digestive function. Stress and anxiety can worsen this by amplifying the mixed signals, making symptoms flare up. Women are more likely to experience IBS, possibly due to hormonal changes affecting gut-brain interactions.
| Gut-Brain Issue | Effect on IBS |
|---|---|
| Misread signals | Pain, bloating |
| Stress triggers | Worsened symptoms |
| Hormonal fluctuations | Increased sensitivity |
| Weak/strong contractions | Diarrhea or constipation |
| Past trauma | Long-term gut disruption |
Identifying trigger foods and managing stress can help, but a proper diagnosis is key to comprehending your unique gut-brain connection.
Dietary Triggers and Stress
Because what you eat and how you feel can have a huge impact on your gut, comprehending dietary triggers and stress is essential for managing IBS. Certain foods—like fried dishes, caffeine, or alcohol—can worsen your symptoms, but triggers vary from person to person.
That’s why personalized dietary management is key. Stress also plays a big role, as anxiety or tension can heighten gut sensitivity, making flare-ups more likely.
Keeping a food journal helps you spot patterns between what you eat, your stress levels, and IBS symptoms. By tracking these, you’ll identify which foods or situations to avoid.
Small changes, like swapping trigger foods for gentler options, can make a big difference in easing discomfort and improving daily life.
Infections and Microbiome Changes
After bouts of food poisoning or stomach bugs, your gut couldn’t bounce back like it used to—and it’s not just bad luck. Infections, especially severe ones, can trigger lasting digestive issues, including IBS.
Even after the infection clears, your gut microbiome—the community of bacteria helping digestion—might stay off-balance, making symptoms like bloating and pain stick around. Childhood infections could also raise your risk of IBS later.
Stress can worsen gut imbalances, creating more symptoms. Lactose intolerance may also become more noticeable, but it’s separate from IBS. While both can cause discomfort after eating, IBS involves broader gut sensitivity, not just an enzyme deficiency.
Managing your gut health with probiotics, fiber, and stress relief could ease these issues.
Causes and Risk Factors for Lactose Intolerance
You could develop lactose intolerance should your body not produce enough lactase, the enzyme that digests milk sugar.
Your genes play a big role, especially in case you’re of Asian, African, or Hispanic descent.
Sometimes, gut issues like infections or celiac disease can also trigger it by damaging your intestines.
Enzyme Deficiency Origins
While lactose intolerance can appear like a simple dairy issue, it actually stems from your body’s struggle to produce enough lactase—the enzyme that breaks down lactose. Without enough lactase, lactose moves through your digestive tract undigested, causing those uncomfortable symptoms like bloating or diarrhea. Here’s what’s happening behind the scenes:
- Primary Deficiency: Most people naturally produce less lactase as they age, especially after childhood.
- Secondary Causes: Conditions like celiac disease or infections can damage your gut, reducing lactase production.
- Medication Side Effects: Some antibiotics or treatments temporarily disrupt enzyme levels.
- Digestive Overlap: When you have IBS, your sensitive gut might react more strongly to undigested lactose.
Your symptoms flare up because your body can’t process lactose, not because dairy is inherently “bad.” Comprehending this helps you manage it better.
Ethnicity and Genetic Links
Lactose intolerance isn’t just about what you eat—it’s also about your genes. Your ethnicity plays a big role because genetic factors determine how well your body produces the lactase enzyme.
Should you be of Hispanic, Asian, or African descent, you’re more likely to lose lactase production after childhood, making lactose intolerance common. Europeans often keep digesting lactose thanks to specific genetic mutations.
Digestive diseases like celiac or Crohn’s can also raise your risk, but that’s different from primary lactose intolerance, which is purely genetic.
While IBS could mimic symptoms, it’s not the same—your genes decide lactose tolerance, not gut sensitivity. Being aware of your family history helps you understand your risk, so you can adjust your diet without guesswork.
Secondary Condition Triggers
Because your gut’s ability to digest lactose depends on more than just genetics, secondary lactose intolerance can sneak up at the time your digestive system takes a hit. Unlike the genetic kind, this type often stems from damage to your digestive tract, reducing lactase production temporarily or long-term.
Here’s what can trigger it:
- Gastrointestinal infections like severe food poisoning or viral gastroenteritis, which harm the gut lining.
- Chronic conditions such as celiac disease or Crohn’s, inflaming your intestines and disrupting lactase.
- Medications like antibiotics, wiping out helpful gut bacteria needed to process lactose.
- Surgeries or trauma to your small intestine, where lactase is made.
The good news?
Once you treat the foundational cause, your lactose intolerance could improve.
Diagnostic Approaches for Each Condition
At the time you’re managing digestive discomfort, figuring out whether it’s IBS or lactose intolerance can feel overwhelming.
For an accurate diagnosis, doctors use different diagnostic approaches. In the case lactose intolerance is suspected, they’ll likely ask about your symptoms after consuming dairy and could suggest a hydrogen breath test to confirm it.
With IBS, there’s no single test—instead, they’ll check whether your symptoms match the Rome IV criteria, like recurring pain and bowel changes over three months. They may also run tests to rule out other conditions.
Since symptoms can overlap, tracking what triggers your discomfort helps. Don’t guess—seek medical advice to pinpoint the issue. Understanding whether it’s IBS or lactose intolerance guarantees you get the right relief.
Dietary and Treatment Strategies for Relief
Should one be managing digestive issues, adjusting your diet can make a big difference—but the approach depends on whether it’s IBS or lactose intolerance. Here’s how to tackle each:
- For lactose intolerance: Skip dairy or try lactose-free alternatives like almond milk. Enzyme supplements can help digest lactose should you indulge.
- For IBS: Track food triggers (like caffeine or fried foods) in a diary and cut them out. Everyone’s triggers differ.
- Experiment gently: Introduce small dietary changes to avoid overwhelming your system.
- Seek balance: Focus on whole, easy-to-digest foods like oats or lean proteins to ease symptoms.